
Enabling secure, compliant, and auditable agent collaboration for prior authorization and beyond — from SimplifyX
As health systems adopt intelligent agents to handle quoting, enrollment, and prior authorization, a new challenge emerges: how do these agents prove their authority, trace their decisions, and comply with regulatory frameworks like CMS, HIPAA, and state DOI rules?
Protocols like MCP and A2A let agents understand and communicate — but they don't define who can act, under what license, or how accountability is enforced.
The Agent Health Insurance Protocol (A2H) solves this.
It's the domain-specific layer that adds identity, authorization, and auditability to every agentic interaction between payers, brokers, providers, and members.
| Layer | Role | Example |
|---|---|---|
| MCP | Context | Agent understands patient data and plan information. |
| A2A | Communication | Provider and payer agents exchange intents, documents, and data. |
| A2H | Compliance & Trust | Every exchange is authorized, credential-verified, and auditable. |
Each agent carries digitally signed credentials — such as:
These credentials are anchored in a verifiable identity registry.
A Health Insurance Mandate is a digitally signed instruction that defines:
Every exchange — whether automated or manual — is packaged in a cryptographically signed A2H envelope, creating a tamper-proof chain of custody.
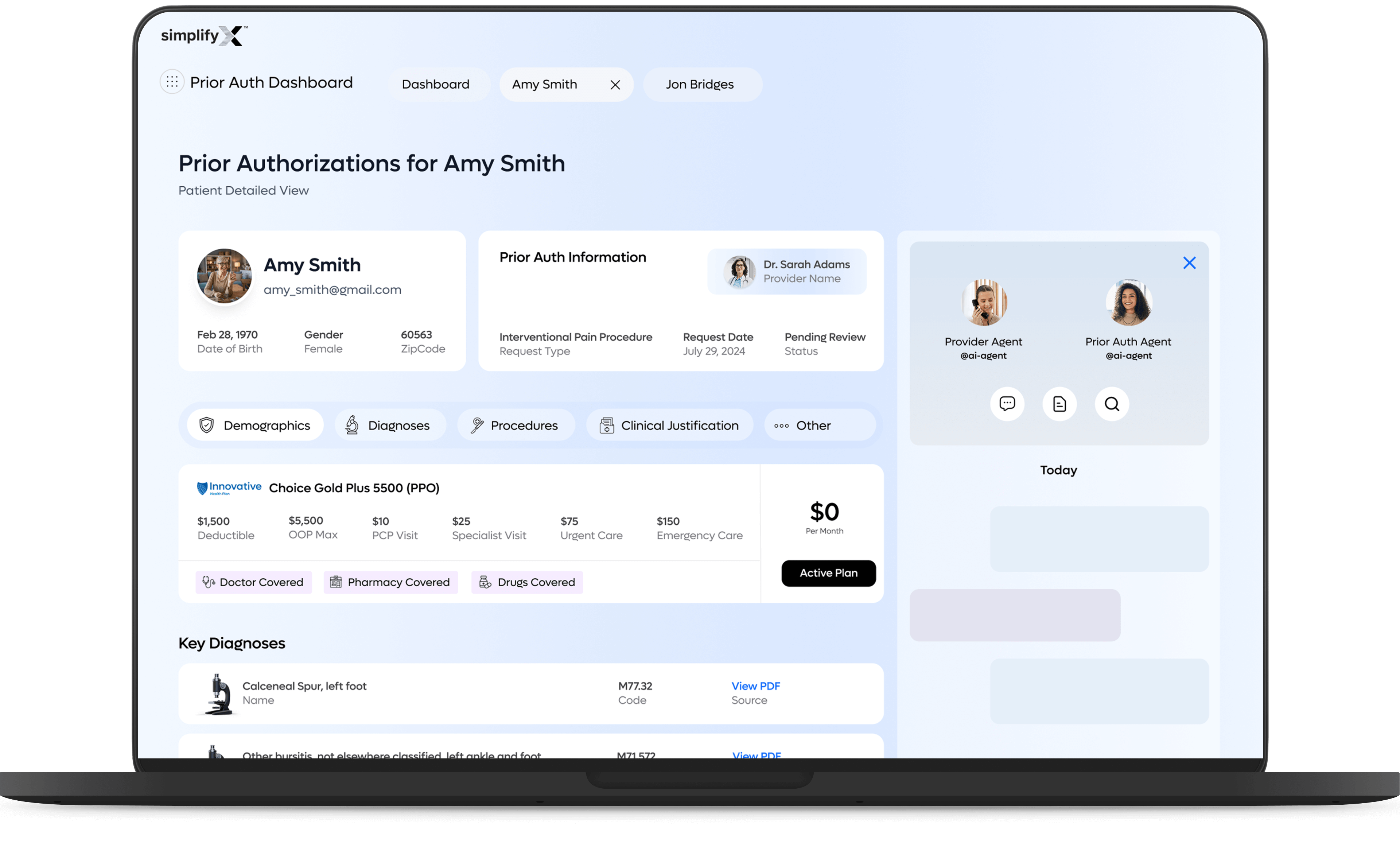
A patient, Amy Smith, is being evaluated for an Interventional Pain Procedure to treat chronic heel and Achilles pain. She is covered under Choice Gold Plus 5500 (PPO) and is treated by Dr. Sarah Adams, an orthopedic specialist.
In the Provider Portal, Dr. Sarah Adams begins a new prior authorization. The system automatically:
Dr. Adams reviews the draft and submits it through her Provider Agent (ProvAgent).
A2H Envelope Example
The Payer Agent (PayerAgent) receives the request and finds the relevant policy: Innovative Policy IPP-2024-07: Interventional Pain Procedures.
Instead of just validating static rules, the Payer Agent performs a contextual policy analysis using the submitted data and generates a criteria map:
| Policy Criteria | Found in Submission | Status |
|---|---|---|
| Diagnosis supported by imaging | MRI report attached | ✅ Met |
| Conservative therapy attempted and failed | Mentioned in note, no duration documented | ⚠️ Incomplete |
| Treatment plan and expected outcomes provided | Missing | ❌ Not found |
Because two of three conditions are not fully satisfied, the payer agent automatically generates a follow-up questionnaire to collect the missing details.
Follow-Up Questionnaire (Auto-Generated by A2H):
These questions are returned to the Provider Agent as an A2H.PriorAuthInquiry message, keeping the conversation structured, auditable, and machine-readable.
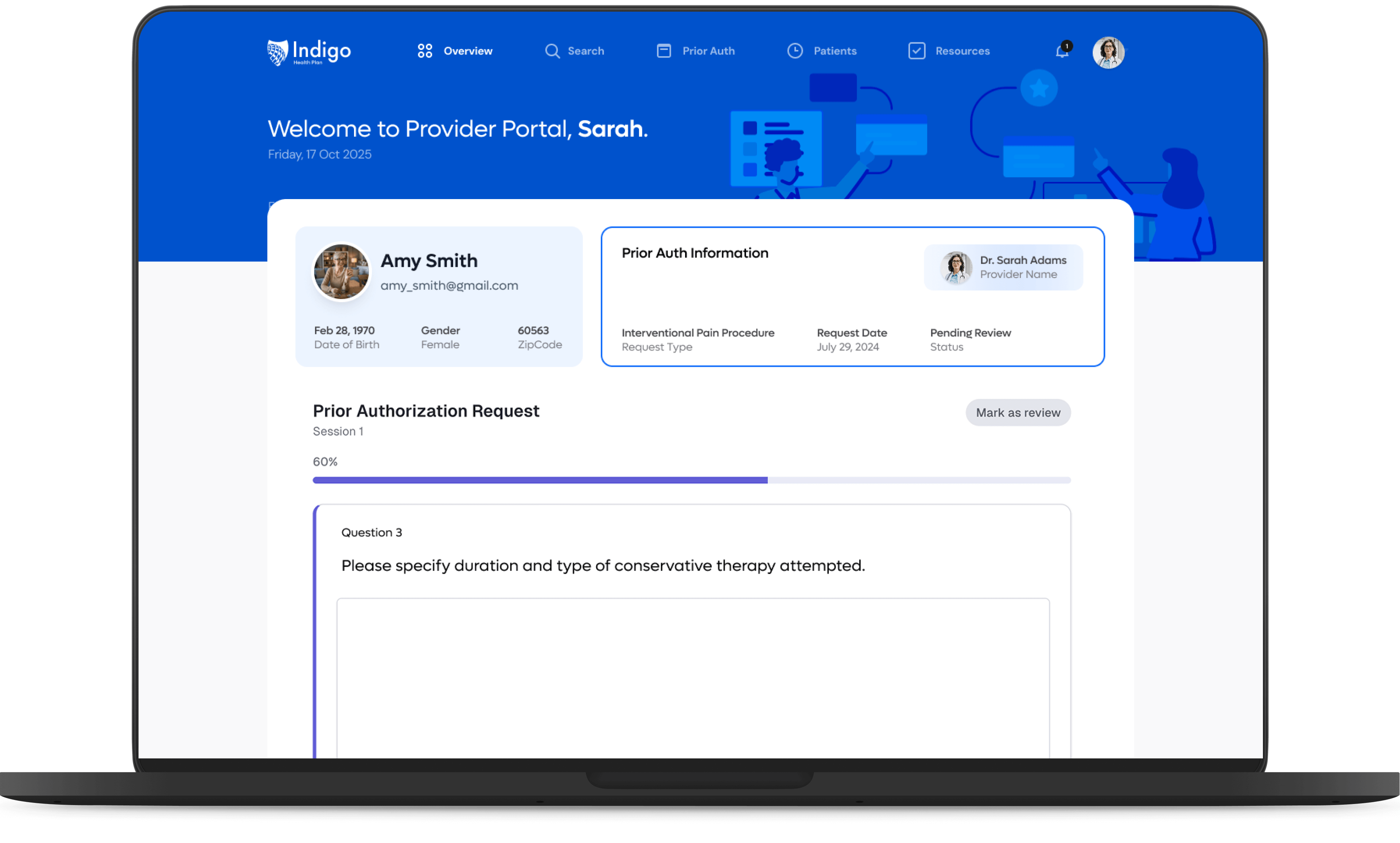
The Provider Agent receives the questionnaire and transforms it into guided Q&A prompts within the Provider Portal:
Dr. Adams fills in the missing information and uploads an updated progress note and therapy record. Each response becomes a verifiable data element linked to the policy criteria that required clarification.
The Provider Agent merges all responses and evidence into an explainable, policy-aligned evidence bundle:
The updated request is resubmitted — still within the same A2H conversation thread — ensuring all actions remain traceable to the original mandate and policy.
On the SimplifyX Payer Dashboard, reviewer Laura Eddy can now see:
If the system determines very high confidence (100%), it auto-approves the request. If further oversight is required (e.g., emerging treatment types like PRP), the case is routed for manual review via an A2H.ManualReviewRequest, assigned to a medical director or nurse reviewer.
Each reviewer action is signed, timestamped, and appended to the same A2H thread — maintaining end-to-end provenance.
The Payer Agent returns a structured A2H.PriorAuthDecision:
The provider sees the final decision in real time — with clear reasoning, policy references, and full traceability back to every question asked and answered.
| Provider Portal | Payer Dashboard (SimplifyX) |
|---|---|
| Guided Q&A + upload workflow | Adaptive questionnaire generation |
| AI assistance for missing info | Confidence-based triage and review routing |
| Real-time submission tracking | Explainable decision tree with evidence links |
| Appeal and re-submit options | Verifiable audit log and reviewer actions |
Together, they form a closed-loop ecosystem — where gaps are automatically identified, follow-up questions are structured, and every decision is explainable, signed, and auditable.
In A2H, manual review isn't a fallback — it's a defined protocol step:
Outcome: Faster decisions, fewer denials, and transparent collaboration between human reviewers and agentic systems.
A2H doesn't replace human judgment — it structures it. Every manual review, rationale, and document is recorded as a verifiable A2H turn with:
| Traditional Prior Auth | A2H-Enabled Prior Auth |
|---|---|
| Fragmented portals and PDFs | Unified agent-to-agent exchange |
| No visibility into policy logic | Transparent criteria and reasoning tree |
| Human follow-up by phone/fax | Automated + human-in-loop collaboration |
| Manual tracking & audit | Cryptographically signed evidence chain |
| Week-long turnaround | Hours or minutes with traceable approval |
Through A2H, SimplifyX shows how providers and payers can collaborate through agents with full traceability and trust. The same digital signature that authenticated the clinician's intent secures the reviewer's decision, creating a single, immutable audit trail from request to resolution.
A2H is the first step toward a world where agents can collaborate across the payer–provider divide with trust, compliance, and full explainability. It turns prior authorization from a black box into a clear, verifiable conversation.

Deepak Bandi leads the vision and execution of the Agentic AI platform that powers enterprise-grade orchestration across industries. With a unique blend of strategic insight and hands-on innovation, he drives the transformation of how systems, agents, and humans work together.